Hematuria is, more often than not, a bad sign.
It’s one of those medical words that sounds curious and distant until it suddenly belongs to you. And you have to define it.
It’s the clinical term for blood in the urine.
It’s a symptom, not a diagnosis.
Below is the timeline of Nathan’s path, from symptoms to treatment up to this point.
A Note, Before I begin this post . . . (tap to Open)
June: The Foreshadowing
It started with me. Like the foreshadowing of a story.
I noticed blood in my urine one morning — no pain, no urgency (common UTI symptoms). Just . . .blood.
A kind of unsettling color in places it doesn’t belong.
I called urgent care, described what I was seeing, and the doctor on the other end didn’t hesitate. “It’s likely cancer. We need to get some labs and—”
Whoa, whoa, whoa. Pull the reins back a bit, I thought.
“What?” I asked. My face turned cold as the blood drained out. I could hear the heartbeat in my ears.
Sheer panic flooded my limbs and body as the provider gave sent me off with an order for labs and a referral to imaging for a CT scan.
I quickly learned that visible blood—gross hematuria—is the primary symptom of urinary tract/bladder cancer; but, cancer is not the primary diagnosis of gross hematuria. Still, I was pretty shook.
After labs and a CT scan, my results came back clean. No infection. No tumor.
Just a kidney stone. I exhaled. It felt like a close call I hadn’t even realized I’d been having.
July: The Symptoms
A few weeks later, Nathan started seeing blood, too.
At first, we didn’t panic. His seemed more concerning, but we convinced ourselves it was probably a stone, or maybe some odd summer dehydration thing. These are the stories you tell yourself to keep breathing.
A couple of weeks later, he passed more blood—this time with tissue. That’s when something in me went still.
September: The Diagnosis
On September 12, Nathan had a cystoscopy—an in office procedure where a small camera is inserted through the urethra to look inside the bladder. Simple, quick, and uncomfortable.
The doctor saw it right away.
A papillary tumor.
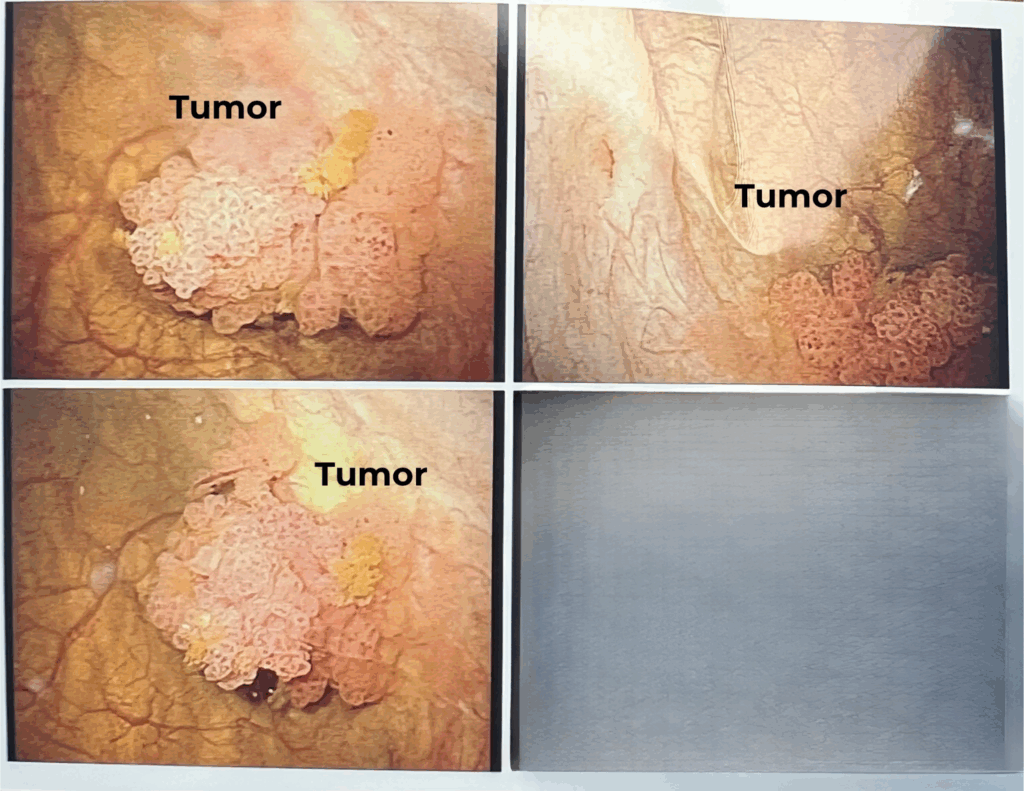
Staging and grading

A week later, the tumor was surgically removed, and pathology confirmed it:
- High-grade urothelial carcinoma
- Aggressive.
- But stage 0—the earliest possible stage!
In stage 0, the tumor is still on the surface and has not rooted into deeper layers or beyond the bladder. That tiny technicality—a millimeter of tissue—can mean everything. The deeper the tumor has grown into the bladder walls, the higher the cancer stage.
Tap to view an image of the tumor
October: Treatment
On Monday, October 27th, Nathan started his first of six treatments. Because the cancer is State 0, his providers recommended an immunotherapy treatment. This treatment is in your bladder to reduce the risk of cancer coming back.
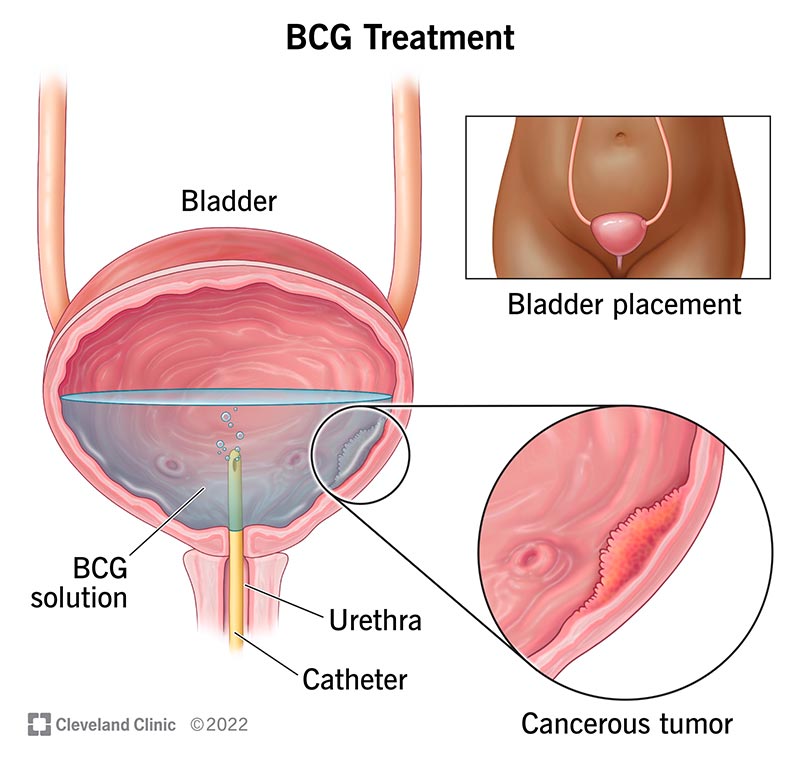
Bacillus Calmette-Guérin (BCG)
Nathan’s providers decided to begin his treatment with immunotherapy. This treatment carries the bacterium BCG and is delivered directly into the bladder through a catheter.
BCG, or BCG therapy, uses the body’s natureal defenses — the power of the immune system — to find and fight cancer cells. It is currently the most common treatment for bladder cancers.
(image via Cleveland Clinic)
BCG BCG is “a strain of Mycobacterium bovis — the same bacterium used to create the tuberculosis vaccine. When used in medicine, Mycobacterium bovis is weakened to reduce harm to the human body.” (source)
Side Effects
Nathan handled the first treatment very well, experiencing nothing more than fatigue for a few days following the treatment.
Nathan continues treatment through December 1. The provider will do another scan at that time. Most likely, they will continue to scan monthly; it is possible, however, that his care team will decide to continue treatments, three weeks every three months until they feel it’s safe to stop.
Next steps
For now, we exhale.
Stage 0 is early. Treatable. Manageable.
But, scans always see more than we ask them to.
In Nathan’s initial bladder CT scan, radiologists noticed a spot on his liver. Upon a closer look in an MRI, that spot was unremarkable; however, another spot was seen on his pancreas. Small, unassuming, tucked away in the shadows of the images. Maybe nothing. Maybe something.
He’s been asked to get an HCC/liver cancer blood screening as well as follow up imaging on his pancreas to “rule out a tumor.
More to sit heavy in the chest.
It’s strange — you think the worst part is hearing cancer.
But sometimes, it’s what comes after.
The follow ups.
The watching.
The waiting.
This is where it started for us—a word, a symptom, a summer that split everything into before and after.
I’ll share what came next soon. It’s still unfolding.
🧐 Curious? 🙋 Have questions?
Do you have questions that weren’t answered in this post? If so, please leave your question in the comments section below, and we will answer. No question is weird or silly; we are happy to share what we’ve learned.